A Case report and literature review: Metachronous tumour in single patient (carcinoma cervix and carcinoma lung)
Dr. Thamizholi S.,1 Pearly Daimari.,2 Balakyntiew Kharshandi.,2
Introduction
In the Era of Advanced diagnostic tools & increased effectiveness of cancer therapy have led to better prognosis of cancer patients. This situation has made the problem of developing subsequent primary tumors more frequent. Literature suggest that the prevalence of multiple primary cancer is estimated between 0.73-11.7% and Incidence increases with age (1).
Cancer survivors are at 14% higher risk of developing second malignancy than general population according to cancer registries in National Cancer Institute. Women had a slightly higher relative risk than men for developing multiple primary malignancy, and most implicated sites were colon, breast, Lung & melanoma of the skin (2).
Despite its low incidence, association of two malignancy is a single patient has been widely reported in the literature. We report a case of 55-year-old women successfully treated by chemoradiation and brachytherapy for squamous cell carcinoma cervix FIGO STAGE IIIB (February 2019) & systemic chemotherapy for 2nd primary Carcinoma Lung STAGE IV (May 2021).
Case presentation
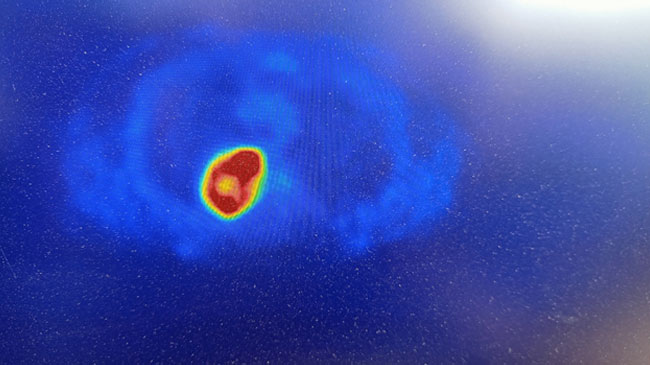
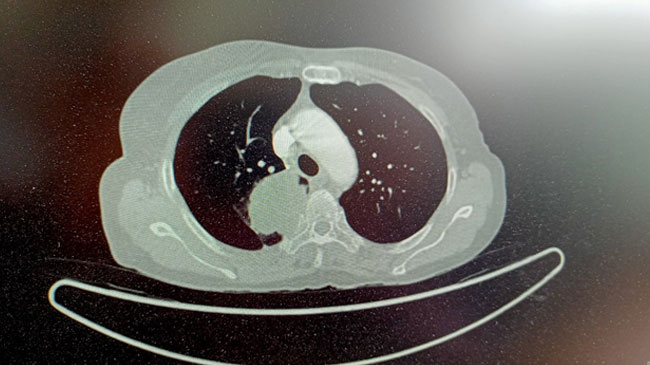
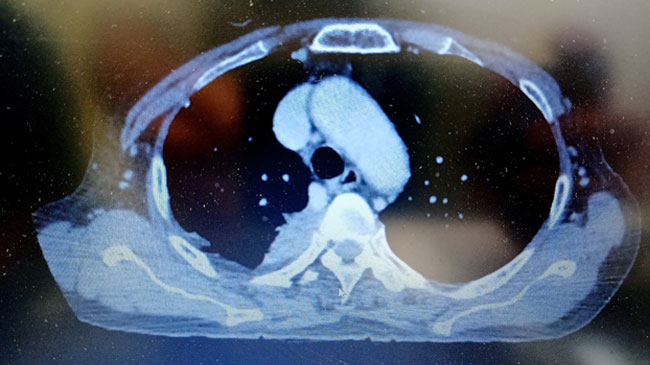
55-year-old women presented with complain of bleeding per vagina for which She was evaluated and diagnosed in December 2018 as squamous all carcinoma cervix STAGE III. She received definitive chemoradiation 46GY/ 23# with concurrent chemo 5 cycles weekly carboplatin under AUC 2 from 18/12/18 to 31/01/2019 followed by ICBT. She was on regular follow up till December 2020. Later she presented with Complaints of upper back pain. She was evaluated for the same. CT Thorax suggestive of right upper lobe lung mass. PET-CT suggestive of metabolically active soft tissue density lesion measuring 67 x 42 x 61 mm involving apical / posterior segment of right Lung upper lobe causing lytic distraction of D2/ D3 vertebrae and right 3rd & 4th rib, extending into spinal canal with thecal sec compression, few lymph nodes at mediastinal station, without metabolic activity, bilateral lung nodules with few of them slowing increase metabolic activity. No definitive scan evidence metabolically active, residual/ recurrent disease at treated bed site in cervix region. CT guided lung biopsy done 06/01/2021. Biopsy suggestive of squamous all carcinomas, IHC → Positive for p16& p40, Negative for TTF- 1 & diagnosed as 2nd primary Carcinoma Lung STAGE IV. She received systemic chemotherapy Paclitaxel 175mg/M2 & carboplatin AUC 5 every 3 weekly for 6 cycles and completed treatment on 26/05/2021. Follow- up CT thorax at the end of 1 Month shows Homogenously enhancing soft tissue thickening, measuring 16x33mm is noted in apical with posterior segment of right upper lobe with sclerosis & erosion of adjacent posterior segment of 3rd, 4th rib. Now she is improved clinically & radiologically with treatment.
Discussion
There are two categories of multiple primary cancer depending on the time of diagnosis of each primary site. Synchronous tumor occurs simultaneously / with interval of six month, while metachronous cancer follow in sequence and more than six months apart (3).
Multiple malignancies are rare & most often involve two sites. cervical cancer is the fourth most common cancer among women, and seventh most common cancer overall worldwide, with an estimated 528,000 new cases in 2012. In India cervical cancer is the second most common cancer among women with estimated 122,844 new cases in 2012 (4).
Cervical cancer patient treated with radiotherapy were at increased risk for second cancer with cancer at heavily irradiated sites (colon, urinary bladder, ovary, Rectum, anus with genital sites) compared to general population (5).
Study from Taiwan's National Health Insurance database observed patients with newly diagnosed cervical cancer between 1997 to 2001. It has found 2004 cancers developed in 35,175 patients with cervical cancer. SIR for all cancer was 1.56 (95% CI, 1.50-1.63, P<0.001). SIR was significantly higher for cancer of uterus (3.76), Lung and mediastinum (2.28), bladder (2.26), bone & soft tissue (2.23) and colon (1.36) (6).
Recently, the occurrence of a second primary malignancy was analyzed in 12048 patients with cervical cancer reported to the Netherlands cancer registry between 1989 to 2008. During the study period, 676 (5.6%) patients were diagnosed with a second cancer. For women aged 50-69 years (the age of our patient when she presented cervical cancer), the SIR of second primary malignancy was 1.8 (95% CI: 1.6-2.0) for all cancer, 1.2 (95%CI:0.8-1.8) for colorectal cancer survivors who underwent radiotherapy were at higher risk for a second tumor when compared to those without radiotherapy (7).
Our patient was 55 years old women who was diagnosed as carcinoma cervix (December 2018) underwent definitive Chemoradiation followed by brachytherapy with 2 year later diagnosed as Carcinoma Lung with same histology Squamous cell carcinoma. IHC -p16 & p40-Positive and TTF-Negative. We consider as 2nd primary Carcinoma Lung Stage IV and she was administered with systemic chemo Paclitaxel & Carboplatin.
Although the mechanism of developing multiple primary cancer remains unclear, several factors have been suspected. Indeed, Smoking, alcohol abuse, previous chemotherapy with or radiotherapy, hormonal Therapy, biological agents with genetic predisposition been to be implicated.
HPV is the primary cause of invasive cervical cancer, and it plays a role in the etiology of cancers of vulva, vagina, anus and a subset of cancer in the oropharynx. Increased risk of HPV-related cancers among cervical cancer survivors may reflect transmission of HPV by sexual behavior to sites other than cervix, a genetic susceptibility to oncogenic effects of HPV, or shared risk factors such as smoking-related cancers (Lung, bronchus, trachea, pharynx, pancreas, and urinary bladder) in patients with cervical cancer treated with or without radiotherapy (5).
Conclusion
Metachronous Tumor in single patient is unusual and the management depends on stages of presentation. Etiology remains controversial in case of two primary with same histology. Still, we need lot more data to analyze and cancer patients must be followed-up for long period of time to understand the development of subsequent malignancy.
References:
1. J.R. Spratt, M.G. Hoag, Incidence of multiple primary cancers per man-year of follow up: 20-year review from the Ellis Fischel State Cancer Hospital, Ann.Surg. 164 (1996) 775–784.
2. R.E. Curtis, D.M. Freedman, E. Ron, L.A.G. Ries, D.G. Hacker, B.K. Edwards, M.A. Tucker, J.F. Fraumeni, New Malignancies Among Cancer Survivors: SEER Cancer Registries, 1973–2000, National Cancer Institute, Bethesda, MD, 2006, NIH Publ. No. 05-5302.
3. H.L. Howe, A review of the definition for multiple primary cancers in the United States, in: Workshop Proceedings from December 4–6, 2002, Princeton, New Jersey Springfield (IL): North American Association of Central Cancer Registries, 2003.
4. International Agency for Research on Cancer WHO. GLOBOCAN 2012: Estimated Cancer Incident, Mortality and Prevalence Worldwide in 2012. http:/globocan.iarc.fr/Pages/fact sheets population.aspx.
5. A.K. Chaturvedi, E.A. Engels, E.S. Gilbert, B.E. Chen, H. Storm, C.F. Lynch, P. Hall, F. Langmark, E. Pukkala, M. Kaijser, M. Andersson, S.D. Fossa, H. Joensuu, J.D. Boice, R.A. Kleinerman, L.B. Travis, Second cancers among 104 760survivors of cervical cancer: evaluation of long-term risk, Natl. Cancer Inst. 99(2007) 1634–1643.
6. C.J. Teng, L.K. Huon, Y.W. Hu, C.M. Yeh, Y. Chao, M.H. Yang, T.J. Chen, Y.P. Hung, C.J. Liu, Secondary primary malignancy risk in patients with cervical cancer in Taiwan: a nationwide population-based study, Medicine (Baltimore) 94 (43) (2015) e1803.
7. M. Arnold, L. Liu, G.G. Kenter, C.L. Creutzberg, J.W. Coebergh, I. Soerjomataram, second primary cancers in survivors of cervical cancer in the Netherlands: implications for prevention and surveillance, Radiother. Oncol.111 (2014) 374–381.
8. J.R. Conner, J.L. Hornick, Metastatic carcinoma of unknown primary: diagnostic approach using immunohistochemistry, Adv. Anat. Pathol. 22 (3) (2015) 149–167.
For Cancer related query call toll free number 18003454325